Does the Gut Microbiome Play a Role in Autoimmune Disease?
on DECEMBER 23, 2014 104 commentsNew research suggests that supporting our gut microbiome may help prevent (and even treat?) autoimmune disease.
 This is a guest post written by staff clinician Amy Nett, MD.
This is a guest post written by staff clinician Amy Nett, MD.Meet your microbiome
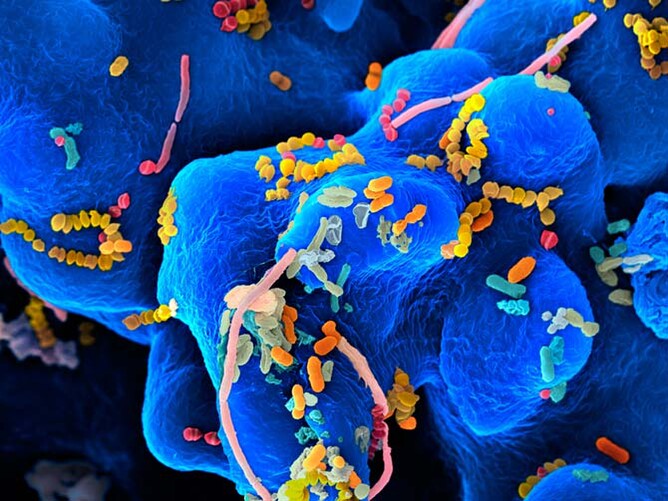
If you commonly read this blog, or listen to Chris's podcast, you have undoubtedly developed an appreciation for the trillions of microbial organisms that normally inhabit a healthy small and large intestine. Most of these microbes are bacteria that have co-evolved with humans, depending on us for their survival just as we depend on them for our health and well-being. For example, we provide nutrients for bacteria which then keep our immune system in check, digest certain carbohydrates that would be indigestible to us, and make vitamins and other important compounds that we would otherwise be unable to produce. This wonderful, symbiotic relationship is what makes up your microbiome. A (hopefully) harmonious collection of microorganisms in our guts that aid in so many of our body's vital functions.The microbiome changes with disease
Our microbiome can affect us in multiple, profound ways ranging from how we store fat (1, 2, 3) to whether we feel happy, anxious or depressed (4, 5, 6). When the normal gut microbial communities are disturbed, whether you've used antibiotics or are suffering from a bacterial infection, it can lead to dysbiosis or small intestinal bacterial overgrowth.Antibiotics, C-sections, poor diet, and autoimmune disease; what's the connection?Dysbiosis is associated with a growing number of diseases such as Crohn's disease (7), ulcerative colitis (8, 9), irritable bowel syndrome (10), and both type 1 and type 2 diabetes (11, 12). You'll find that the variety and balance of gut bacteria is often different in patients with chronic inflammatory conditions as compared with healthy individuals. Research now suggests that these diseases are not due to any single bacterium, but from changes to the entire microbiome. And since a large part of our immune system is found within the gut, several diseases resulting from dysbiosis are autoimmune diseases.
What is autoimmune disease?
Autoimmune disease can be thought of as a case of mistaken identity: the immune system targets normal proteins as if they were harmful foreign invaders and becomes overactive. Normally, the immune system responds to a specific pathogen, like a cold virus, and once that pathogen is cleared, the immune system can settle down to its normal state. In the case of autoimmune disease, the immune system often stays on high alert, resulting in chronic inflammation.With more than 80 different types of autoimmune disease, this class of disease has been particularly difficult to understand: what exactly causes the immune system to attack otherwise normal healthy human cells?
The three legged stool of autoimmune disease.
Dr. Alessio Fasano, a world-renowned gastroenterologist, expert in autoimmune disease, and pioneer in understanding celiac disease, describes autoimmunity as a three-legged stool, meaning that three essential components must be present in order for someone to develop an autoimmune disease:- Genetic predisposition: certain genes make individuals more likely to develop certain diseases.
- A trigger: specific antigen, or protein, that the immune system recognizes as a threat (real or not), that sets off the cascade of over-activation. In the case of celiac disease, the trigger is gluten. However, in the vast majority of autoimmune diseases the trigger remains unknown.
- Intestinal permeability (also referred to as "leaky gut"): this increased permeability means that the normally tightly knit cells of the intestines are weakened and "leaky". This allows large compounds, such as proteins from food or bacteria, entry into our bloodstream. Leaky gut can occur due to any number of reasons such a food sensitivities, gut infections, or chronic stress.
Does the microbiome play a role in autoimmune disease?
Increasing attention is being paid to the importance of the microbiome in health and disease—even slight imbalances have far reaching consequences. It has become clear that the microbiome profoundly affects our immune system, and new research provides insights into how changes in the microbiome can act as the trigger in developing autoimmune disease.A recent paper reviewed some of the most recent research that the health of our microbiome may be the key factor in whether or not we develop an autoimmune disease (13). Below are a few of the key points:
Two of the most significant autoimmune diseases in terms of global morbidity and mortality are Type 1 diabetes mellitus, and rheumatoid arthritis (RA).
Type 1 Diabetes Mellitus
Type 1 diabetes (T1D) is an autoimmune disease with antibodies that destroy the insulin-producing cells of the pancreas, leading to insulin deficiency and blood sugar irregularities. Most often patients are diagnosed in childhood or adolescence, and there is a known genetic association. However, in studies with twins (who share the same genes), only about 50% of twins both go on to develop the disease. This further supports the idea that the development of disease depends on more than genes alone. For instance, immigrants have a risk of developing T1D that is dependent on their place of residence, not their country of origin.Studies looking at differences in the gut microbiome between people with T1D and healthy individuals have found the following differences:
- Children with T1D have a smaller amount of beneficial bacteria.
- Children with T1D have less stability and diversity of bacteria in their gut.
- There are significant differences in both bacterial composition and metabolic capabilities between those with T1D and without.
- After treatments to normalize blood sugar in T1D patients, there was also a return to microbial diversity in those individuals.
Rheumatoid Arthritis
Rheumatoid arthritis affects about 1.5 million people in the United States, and up to 1% of adults worldwide. It is an autoimmune disease that affects many of the joints throughout the body, most commonly the joints of the wrists and hands.As with T1D, there is a known genetic association. However, studies with twins again prove that genes play even less of a role in the development of RA when compared with T1D. Research again supports a relationship between the microbiome and the development and progression of RA. Of particular interest is the role of the bacteria living in ones mouth.
Periodontal disease and RA
- Patients with newly diagnosed RA have higher rates of severe periodontitis and more tooth loss despite normal oral hygiene compared to healthy individuals.
- The severity of a patients periodontal disease can be correlated with the severity of their RA disease activity.
- Specific bacteria that live in the mouth have been shown in animal models to increase the severity of joint disease.
- Specific bacteria are present in both dental plaque of patients with RA, and in joint fluid.
One more reason to take care of your gut?
As if we didn't already have enough reasons to take care of our gut and help our beneficial bacteria thrive, it may be that decreasing our risk of developing an autoimmune disease is one more important reason to be good to your microbiome.Now I'd like to hear from you: Have you made changes in your diet or gut health that have affected your autoimmune disease? Do you notice flares or exacerbations of your autoimmune disease when you eat certain foods?
 About Amy: Amy Nett, MD, graduated from Georgetown University School of Medicine in 2007. She subsequently completed a year of internal medicine training at Santa Barbara Cottage Hospital, followed by five years of specialty training in radiology at Stanford University Hospital, with additional subspecialty training in pediatric radiology.
About Amy: Amy Nett, MD, graduated from Georgetown University School of Medicine in 2007. She subsequently completed a year of internal medicine training at Santa Barbara Cottage Hospital, followed by five years of specialty training in radiology at Stanford University Hospital, with additional subspecialty training in pediatric radiology.Along the course of her medical training and working through her own personal health issues, she found her passion for functional medicine, and began training with Chris in June of 2014. She has recently joined his clinical practice to work with patients through a functional medicine approach, working to identify and treat the root causes of illness. Similar to Chris, she uses nutritional therapy, herbal medicine, supplements, stress management, detoxification and lifestyle changes to restore proper function and improve health.
Like what you've read? Sig